Ovarian cancer remains one of the deadliest forms of cancer, particularly the high-grade serous ovarian carcinoma (HGSOC), which often evades detection until it reaches advanced stages. Recent research utilizing murine models has illuminated a potential breakthrough in our understanding of this devastating disease. The study, spearheaded by pathologist Alexander Nikitin from Cornell University, has led to the identification of specific cellular precursors in the oviducts of mice that may play a crucial role in the development of HGSOC. If these findings hold true in humans, they could pave the way for earlier diagnoses and more effective treatments.
High-grade serous ovarian carcinoma accounts for a significant percentage of ovarian cancer cases and is particularly aggressive. Alarmingly, statistics indicate that approximately 80 percent of HGSOC cases are diagnosed at an advanced stage, where therapeutic alternatives are severely limited. The five-year survival rate post-diagnosis remains starkly low, highlighting the urgent need for strategies aimed at earlier detection. Previous research has suggested that many of these cancers may originate in the fallopian tubes rather than the ovaries, shifting the focus and methodology of ongoing research.
For a decade, scientists have scrutinized the fallopian tubes and observed lesions with genetic connections to ovarian tumors. However, despite the progress made in this arena, there remains a critical gap in knowledge regarding which specific cell types are responsible for initiating HGSOC. This gap has been constraining efforts to establish new diagnostic markers that could herald earlier intervention and potentially improve patient outcomes.
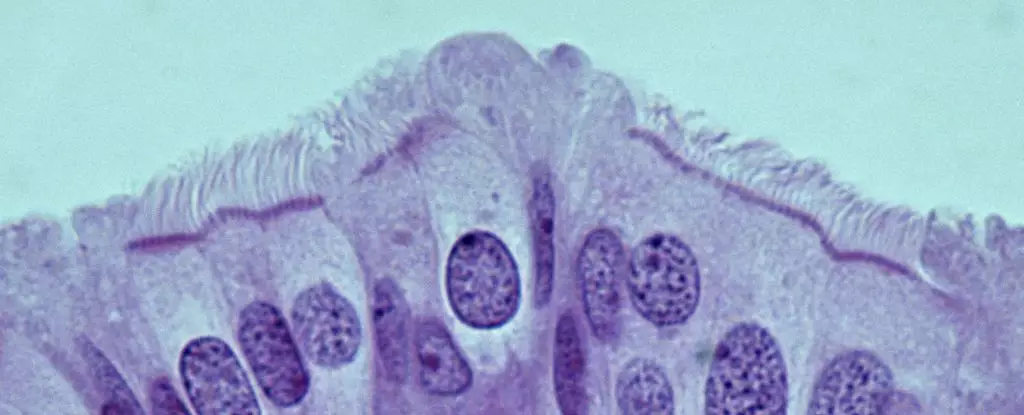
The latest study undertaken by Nikitin and his team provides compelling insights into the cellular landscape of the oviduct. For the first time, researchers have meticulously cataloged the various cell types within this area, offering a much-needed perspective on their contributions to ovarian cancer. The surprising outcome was the identification of pre-ciliated cells as the primary culprits for cancer development, a shift from the previously held assumption that stem cells would be the most cancer-prone.
Pre-ciliated cells are transitional entities in the pipeline toward maturation into fully ciliated cells, known for their role in propelling oocytes through reproductive tracts. The study uncovered a significant link between two genetic mutations associated with HGSOC and the behavior of these pre-ciliated cells, suggesting that when these mutations are present, they drastically accelerate the process of cancer formation within these cells. This connection hints at a complex relationship between the regulation of cilia formation and the onset of ovarian cancer, opening avenues for further investigation into both genetic and non-genetic factors involved in disease progression.
The implications of these findings extend beyond HGSOC alone and may resonate with other forms of malignancy, such as pancreatic cancer, which has been similarly linked to irregularities in ciliogenesis. The tantalizing prospect of identifying specific cancerous precursors within human tissue could fundamentally change the landscape of early detection methodology in oncology. The inherent challenges in translating these findings from murine models to human counterparts remain, but the potential for breakthroughs in diagnostic approaches is clear.
The necessity of further studies cannot be overstated. Future research is essential to unravel not only the mechanisms that lead to ovarian tumor formation but also to investigate whether other genetic mutations related to HGSOC exhibit comparable or divergent effects. By expanding the knowledge base around these critical cellular dynamics, researchers stand poised to develop targeted therapies and improved screening protocols.
The study by Nikitin and his team underscores a transformative moment in the fight against ovarian cancer. By shining a light on the pre-ciliated cells of the oviduct as key players in the disease’s outset, we inch closer to unlocking the secrets of HGSOC. The ultimate goal remains clear: to shift the paradigm toward early detection and proactive treatment, thereby improving survival rates and the quality of life for those affected by this aggressive malignancy.

Leave a Reply