Aging is a compelling and complex biological process that instigates a multitude of changes within our bodies, particularly concerning health. One of the most intriguing paradoxes is the dual nature of cancer risk as we age. For individuals in their 60s and 70s, there is a notable increase in the risk of developing cancer, primarily due to the accumulation of genetic mutations over the decades. However, this trend appears to reverse after reaching the age of approximately 80, leading scientists to question the underlying mechanisms. Recent research exploring the changes in cellular characteristics during aging has shed light on this phenomenon, revealing essential information that may significantly influence cancer treatments and prevention strategies.
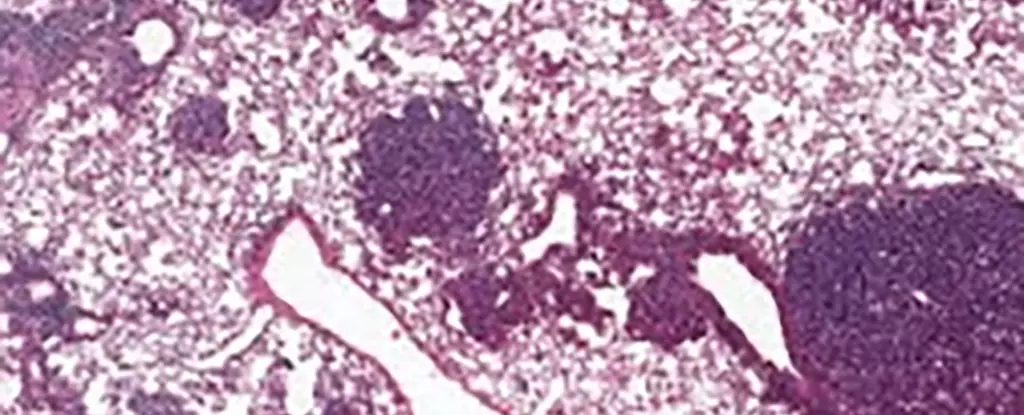
A recent international research collaboration provided groundbreaking insights into lung cancer, specifically the behavior of alveolar type 2 (AT2) stem cells, which are critical for lung health and regeneration. AT2 cells are known to serve as the breeding ground for many forms of lung cancer, making them a focal point for understanding cancer dynamics in older populations. In their study, scientists tracked the changes in these cells in both mice and human samples and discovered a startling connection between aging, cellular iron levels, and the development of cancer.
A significant finding emerged concerning a protein known as NUPR1. The data indicated that older mice exhibited higher concentrations of NUPR1, leading to a cellular response akin to an iron deficiency. Interestingly, the aging cells had more iron than their younger counterparts, but they were exhibiting dysfunction that inhibited cellular renewal—the very mechanism that fuels both regeneration and tumor growth. This paradox raises important questions regarding how the aging process influences cellular metabolism and promotes cancer resistance.
An intriguing aspect of this research lies in the potential therapeutic avenues that might arise from understanding NUPR1’s role in iron metabolism. Targeting iron levels in older adults could serve as a means of enhancing lung regeneration, especially in patients recovering from conditions like long-COVID. By artificially lowering NUPR1 levels or increasing available iron, researchers found a notable improvement in cell growth capabilities. These findings suggest a new frontier for therapeutic interventions that could restore functionality to aging cells, with significant implications for managing cancer in older populations.
Moreover, the results have implications for the emerging field of ferroptosis-based cancer treatments. Ferroptosis is a specific form of cell death triggered by elevated iron levels, and its efficacy appears to decline in older cells. The insights gathered from this research indicate that older cancer patients may respond differently to ferroptosis inducers, suggesting that timing and age should not be overlooked when developing and applying such therapies. More research is needed to understand the complex relationship between iron metabolism and cancer treatment outcomes thoroughly.
The research not only emphasizes the significance of cellular changes in older ages but also highlights the urgent need for preventive measures among younger individuals. Experts involved in this study assert that the detrimental events leading to cancer, often instigated by lifestyle choices such as smoking or excessive sun exposure, are significantly more perilous in youth. This reaffirms the critical role of preventive healthcare, advocating for education and interventions aimed at young adults to deter behaviors that increase early cancer susceptibility.
As we dig deeper into the mechanisms of aging and cancer biology, there remains a vast landscape of unanswered questions. While this study offers various insights into the intricate relationship between age, cellular function, and cancer risk, it also points to the pressing need for personalized treatment strategies. Each patient’s unique circumstances, including cancer type, stage, and age, must be accounted for in order to cultivate effective treatment paradigms.
Understanding the nuanced dynamics between aging and cancer opens the door to innovative research and clinical applications. The studies conducted on AT2 stem cells and their connection with NUPR1 and iron regulation not only provide fundamental insights into the biology of cancer but also pave the way for developing tailored treatment approaches that could significantly benefit aging populations. There’s still much to explore in this evolving field, as the aging process continues to challenge our understanding of health and disease.

Leave a Reply