The relationship between antibiotic use and cognitive decline, particularly dementia, has garnered significant attention in recent years. While some studies suggest a potential link, particularly highlighting the disruption of the gut microbiome caused by antibiotics, recent findings from the ASPREE trial present a more nuanced view. With over 4.7 years of follow-up involving 13,500 seniors, researchers conclude there is no substantial connection between antibiotic usage and an increased risk of dementia in healthy older adults. However, this assertion is fraught with complexities that merit careful consideration.
The ASPREE (Aspirin in Reducing Events in the Elderly) trial aimed to determine the effects of low-dose aspirin on health outcomes in older adults without serious illness. As part of the study’s extension, researchers evaluated the implications of antibiotic prescriptions and cognitive performance among participants. The primary investigators, led by Andrew Chan, MD, MPH, at Harvard Medical School, assessed cognitive decline using comprehensive tests measuring various cognitive functions such as episodic memory and executive function.
Of the participants, a notable 62.5% received at least one antibiotic prescription during the study period. The results indicated no significant relationship between antibiotic use, either in frequency or type, and the onset of dementia or cognitive impairment. Specifically, the hazard ratios calculated suggested a reassuring picture for clinicians prescribing antibiotics to older adults, as potential detrimental effects on cognitive function were not observed.
Despite these positive findings, the body of research on antibiotics and cognitive health is far from unanimous. Previous investigations, such as the Nurses’ Health Study II, revealed concerning associations, where midlife women exposed to antibiotics for at least two months exhibited lower cognitive performance several years later. Furthermore, earlier randomized trials presented paradoxical results, leading to confusion in the scientific community.
This juxtaposition of findings highlights a critical aspect of scientific research—the need for replication and diverse study designs. While the ASPREE study represents a significant addition to the literature, it is vital to approach its conclusions with a healthy skepticism. Critics, including Wenjie Cai and Alden Gross from Johns Hopkins University, have emphasized the necessity for cautious interpretation of these results, particularly noting the specific health profiles of the participants.
A critical aspect of understanding the implications of the ASPREE trial findings is acknowledging their limitations. Participants in the study were primarily healthy older adults who did not have prior cognitive impairments, suggesting that these results may not be broadly applicable to the general aging population, which often includes individuals with diverse health conditions and pre-existing cognitive challenges.
Moreover, the reliance on filled prescriptions as an indicator of antibiotic use may not accurately reflect actual consumption. Some individuals may have filled prescriptions but failed to take the medication, while others might use antibiotics acquired through informal channels or other means. This potential underreporting complicates the understanding of the direct effects of antibiotics on cognition.
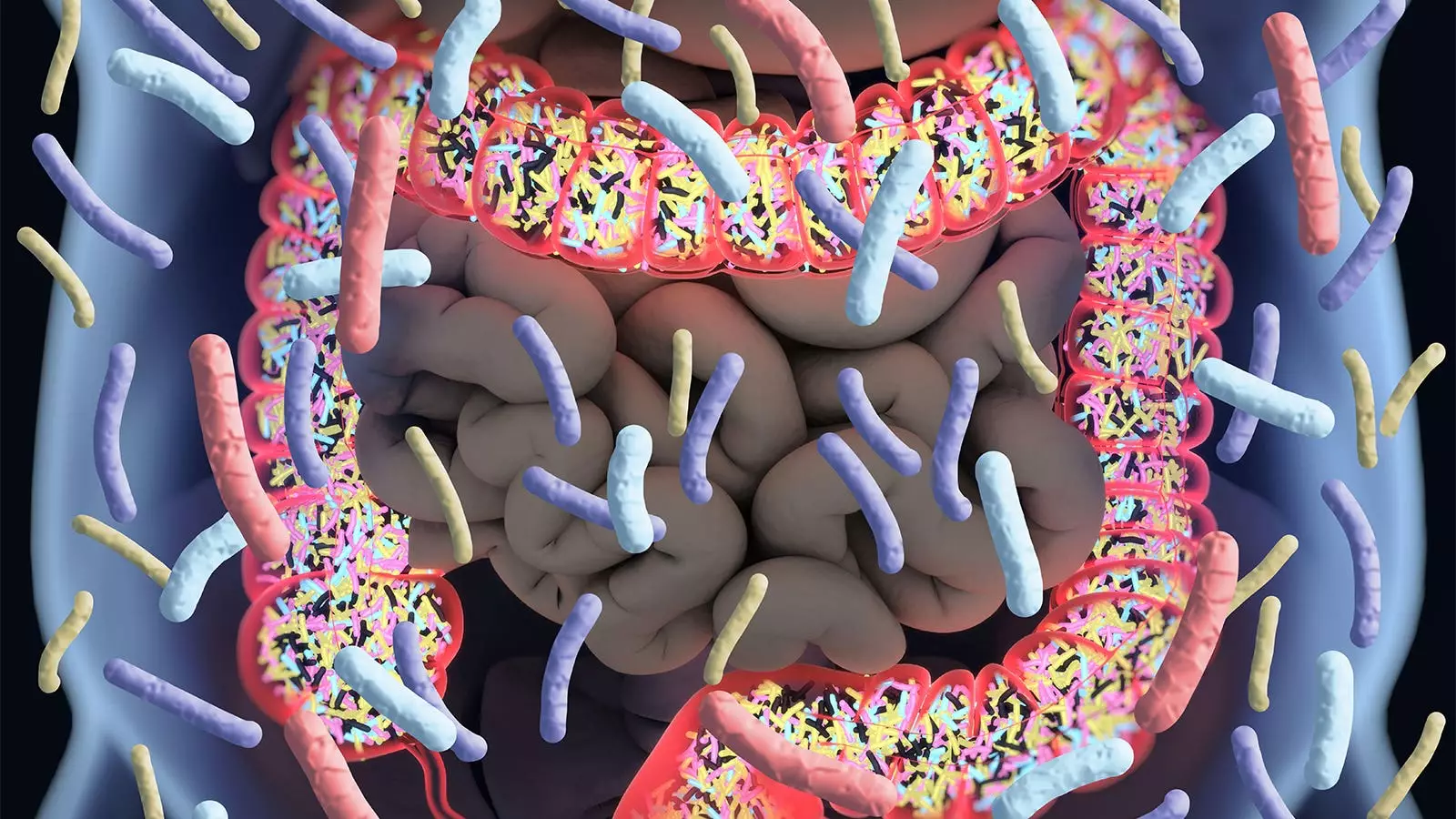
The implications surrounding the gut microbiome’s involvement in cognitive health cannot be overlooked. Chan and colleagues have raised relevant concerns that antibiotic treatment can alter gut flora, which plays a crucial role in maintaining overall health, including cognitive function. While this study provides some reassurance regarding antibiotic use in a specific cohort, the larger question of long-term consequences on the microbiome, particularly in the context of cognitive decline, remains unresolved.
From a clinical perspective, the application of these findings may be limited in practice. Healthcare providers, while reassured about prescribing antibiotics to healthy older adults, must remain vigilant regarding patients with complex health profiles. Future research should expand to include more diverse populations and examine the multifaceted relationships between antibiotic use, microbiome health, and cognitive impairment.
The ASPREE trial has contributed valuable knowledge to the discussion surrounding antibiotics and cognitive health. However, as with all scientific findings, caution is necessary when evaluating their applicability to broader populations. As the debate continues, one thing remains clear: understanding the intricate connections between medication, health, and cognition requires ongoing research and careful analysis. Only through rigorous and diverse studies can we hope to unravel the complexities of how antibiotics may impact cognitive health across varying populations.

Leave a Reply