In recent months, the World Health Organization’s stark warning about a looming chikungunya epidemic should serve as a clarion call to every responsible stakeholder—governments, communities, and global health organizations alike. The signs are eerily reminiscent of the early 2000s outbreak, a grim reminder that history tends to repeat itself when preparedness falters. This isn’t merely about health; it’s about a collective failure to heed the lessons of the past. The threat is palpable, and the consequences, potentially devastating, demand unwavering attention and resilience.
As climate change fuels the expansion of Aedes mosquitoes—those tiny but lethal vectors—the threat transcends tropical zones, inching into temperate regions where populations are less immune and less prepared. The pattern of rapid, uncontrolled spread, as witnessed in the Indian Ocean islands, underscores the pressing need for a comprehensive, forward-looking response. Yet, the global community remains predominantly reactive rather than proactive, bogged down by bureaucratic inertia and a reluctance to prioritize public health. This apathy, whether deliberate or due to misinformation, could turn a manageable outbreak into a catastrophe that overwhelms healthcare systems.
The Hidden Danger of Underestimation and Misdiagnosis
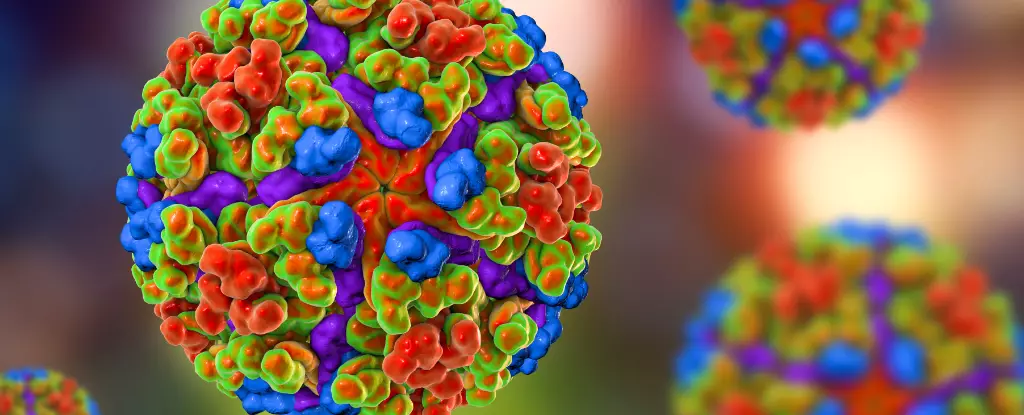
Chikungunya’s resemblance to other arboviruses like dengue and Zika camouflages its true threat. Its symptoms—fever and debilitating joint pain—are deceptively benign at first glance, often leading to delayed diagnosis and treatment. This stealthy nature hampers swift containment efforts, allowing the virus to spread silently within communities. Such misdiagnosis is not a trivial issue; it’s a breach of our collective defense system that could lead to unchecked transmission, especially in regions with weak healthcare infrastructure.
Moreover, the perception that chikungunya is a “lesser” threat is dangerously misleading. The case fatality rate, whispered at less than one percent, obscures the grim reality—when millions are infected, hundreds or even thousands could succumb. This is not just about morbidity but about the disproportionate impact on the most vulnerable—poor, underserved, and often ignored populations. Their voices remain unheard amid the din of global priorities, yet their suffering underscores the ethical imperative for immediate action.
Climate Change: The Catalyst for a Deadly Spread
The expansion of Macau Aedes albopictus, or the tiger mosquito, is a chilling symptom of a planet on a destructive trajectory. Warming temperatures facilitate the breeding and migration of these vectors into new territories, and with them, the viruses they carry. The geopolitical implications of this are profound; it’s not merely about health but about environmental policies, urban planning, and global cooperation. We are witnessing a biological consequence of humanity’s reckless disregard for the planet, and the bill is coming due in the form of outbreaks that threaten to spiral out of control.
This environmental shift amplifies the inequality in our global health responses. Wealthier nations with advanced healthcare and surveillance capabilities can mitigate some risks, but poorer regions—where infrastructure is fragile—sit at the mercy of a virus that spreads faster than policy responses can adapt. The stark reality is that climate change isn’t a distant threat; it is actively fueling the next wave of epidemics, and our inaction right now may condemn millions to avoidable suffering.
A Critical Need for Paradigm Shift in Public Health Strategies
The reality is this: conventional approaches to epidemic prevention are inadequate in a rapidly changing world. The WHO’s call for urgent preparedness is justified, but it must be expanded into a broader, more integrated strategy that prioritizes early detection, community engagement, and global cooperation. Relying solely on individual protective measures—like mosquito repellents and stagnant water management—is insufficient without systemic support.
We must advocate for stronger health systems, better surveillance, and innovative vector control methods. Public awareness campaigns should not be passive; they must actively challenge complacency and misinformation. Governments need to view health security as a fundamental component of sustainable development, not an expendable luxury. The entire global community must recognize that neglecting the threat of chikungunya and other vector-borne diseases risks unleashing a cycle of pandemics that can destabilize economies and threaten social stability.
By critically examining our current approach, it becomes clear that waiting for a full-blown crisis is no longer acceptable. Bold, decisive action rooted in science, equity, and foresight is overdue. Ignoring this warning is tantamount to inviting catastrophe—one that, once unleashed, will be far-reaching and profoundly devastating.

Leave a Reply