The prevalence of pediatric obesity has emerged as a significant public health concern, prompting professionals in the healthcare sector to seek effective treatments and interventions. With an increasing number of youngsters facing obesity-related health issues, the introduction of GLP-1 receptor agonists, particularly liraglutide, presents both a hopeful and cautious narrative. As a pediatric obesity medicine specialist, I have confirmed the beneficial effects of such medications in adolescent populations, yet the need for critical examination remains, especially concerning younger children who are often left without viable pharmacological options.
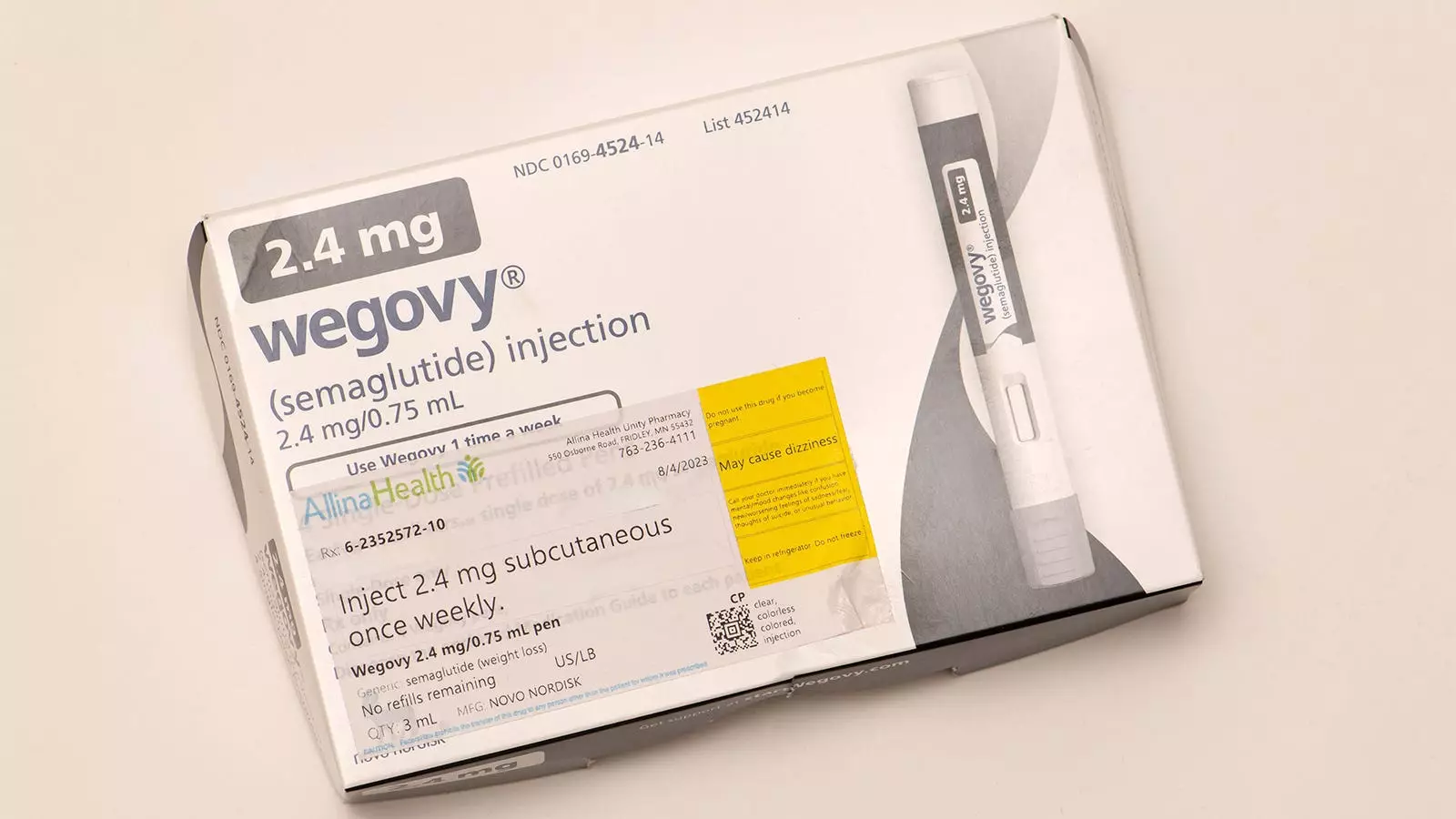
Childhood obesity is not just a cosmetic issue; it poses serious health risks such as diabetes, cardiovascular problems, and psychosocial challenges. The treatment of adolescent obesity using GLP-1 receptor agonists, particularly semaglutide (Wegovy), in conjunction with comprehensive lifestyle interventions has produced encouraging outcomes. These interventions have been linked to improvements in several areas, including increased physical activity, enhanced sleep quality, better body image perception, and increased self-confidence.
However, the situation for younger children, particularly those under the age of 12, remains starkly different. Currently, there are no pharmacological treatments approved for this age group despite the alarming rates of obesity in children, which can lead to medical complications such as prediabetes, fatty liver, and sleep apnea. The lack of effective treatment options in this vulnerable population creates an urgent need for evolving treatment protocols and the exploration of medications like liraglutide.
Recently, the FDA has begun evaluating liraglutide’s potential approval for treating severe obesity in children aged 6 to 12. This decision is grounded in a pivotal randomized trial documented in the New England Journal of Medicine (NEJM) that underscored liraglutide’s safety and efficacy. In the trial involving 82 children, those receiving 3 mg of liraglutide alongside lifestyle interventions showed significant improvements, including a decrease in BMI. However, it is crucial to highlight that gastrointestinal side effects were prominent among the treatment group—80% of participants reported mild to moderate effects.
The American Academy of Pediatrics has endorsed considering weight loss medications for children ages 8 to 11 if aligned with established guidelines on risks and benefits. However, before I would implement this approach, the necessary FDA approval must be secured, and even then, careful deliberation is warranted.
As we delve into the potential advantages of liraglutide, it is critical to approach from a risk-benefit perspective. The potential benefits include:
1. **BMI Reduction**: The possibility of observing modest reductions in BMI during treatment may assist in mitigating the associated risks of obesity.
2. **Metabolic Benefits**: Although the initial trial did not yield statistically significant improvements in key metabolic risk factors, trends suggest potential therapeutic effects.
3. **Psychosocial Implications**: Insights from studies targeting adolescent populations taking obesity medications have indicated possible benefits in psychosocial aspects, which merits further exploration in younger cohorts.
Conversely, the risks associated with liraglutide treatment cannot be overlooked:
1. **Long-Term Safety Concerns**: The long-term implications of liraglutide usage in children, specifically concerning growth and adult height, remain uncertain.
2. **Side Effects**: The spectrum of side effects, some of which may not be discovered until the medication is more broadly used, poses a potential risk.
3. **Weight Rebound**: Notably, when the medication is discontinued, participants often experienced significant weight gain. In the NEJM trial, after a six-month cessation, participants gained back nearly all the lost weight, indicating the transient nature of pharmacological interventions.
4. **Compliance Issues**: The necessity of daily injections raises concerns about adherence and the potential for psychological resistance among young patients and their families.
The landscape of treating childhood obesity is evolving but remains fraught with complexities. Severe obesity is a multifaceted disease requiring tailored, individualized treatment approaches. While the potential approval of liraglutide for children brings a glimmer of hope, it is a double-edged sword. My position remains that the risks typically outweigh the benefits in most cases for children under 12.
However, should liraglutide gain FDA approval, it will signify progress toward addressing obesity in children in a more inclusive manner. The integration of pharmacological treatments should be accompanied by intensive lifestyle interventions, and ongoing dialogue with parents and caregivers will be paramount. As further studies pave the way for a comprehensive understanding of obesity management in children, we must remain cautiously optimistic and ensure that the health of our youngest populations is prioritized above all.

Leave a Reply