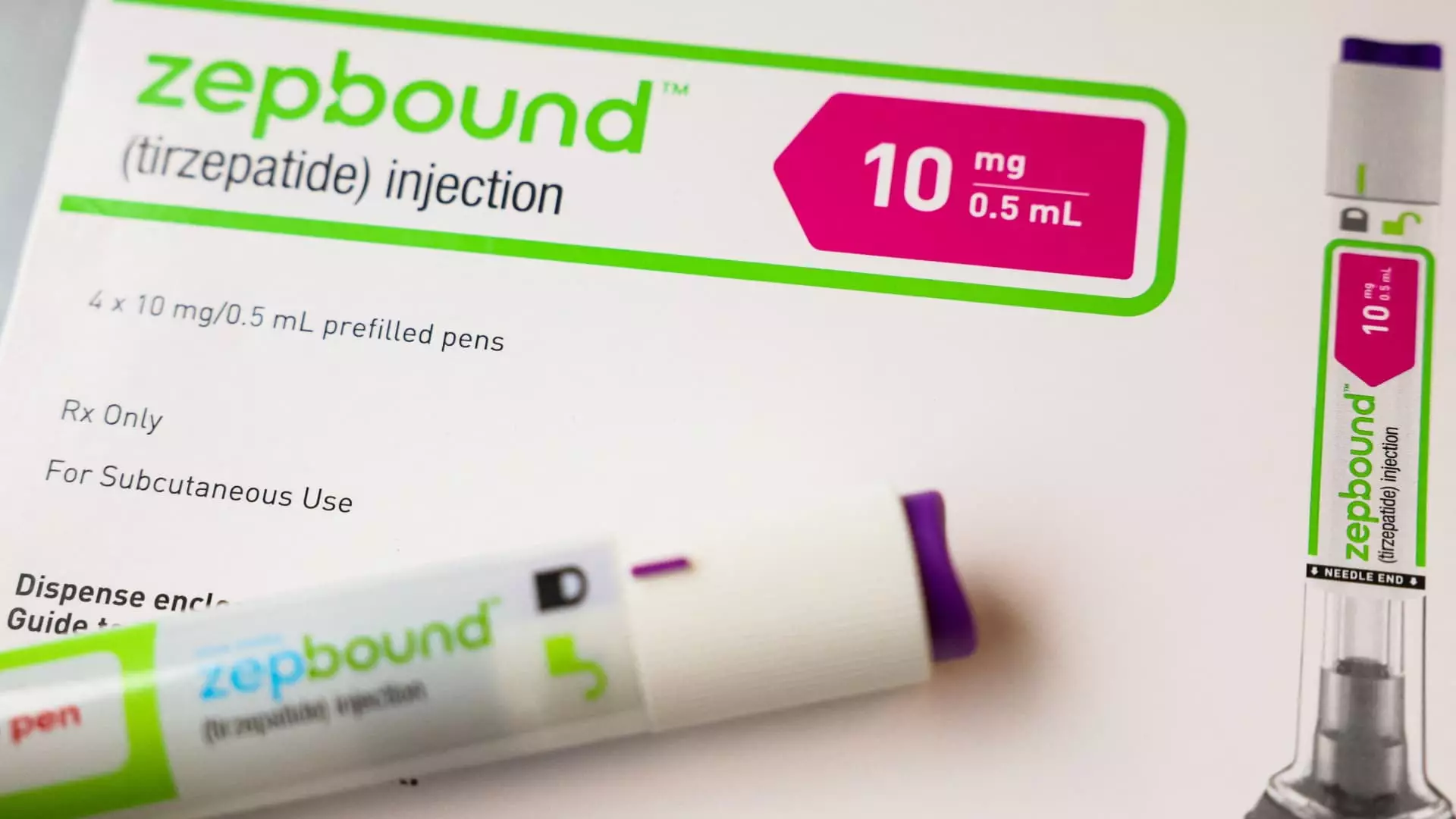
In a significant development for the healthcare landscape, Medicare has begun to cover Eli Lilly’s groundbreaking obesity treatment, Zepbound, specifically for obstructive sleep apnea (OSA). This decision marks a pivotal moment in the way Medicare interacts with obesity medications, which have historically faced scrutiny when it comes to insurance coverage. Despite Zepbound’s formidable price tag of approximately $1,000 prior to insurance, the demand for this injectable therapy has surged over the past year, highlighting the increasing public interest in effective weight management solutions paired with related health conditions.
Zepbound received FDA approval for the treatment of OSA, a condition affecting an estimated 20 million Americans characterized by intermittent breathing during sleep due to obstructions in the airway. This approval not only highlights the drug’s novel mechanism but also its dual purpose, enabling its coverage under Medicare Part D plans. However, this coverage is subject to a stringent set of conditions, including the requirement that the medication be used for an FDA-approved indication, thus creating additional layers of complexity for patients seeking access.
According to a statement from the Centers for Medicare & Medicaid Services (CMS), Medicare can only accommodate obesity drugs if they serve a dual purpose beyond weight management. This means that prescribers must demonstrate a clear medical necessity for the drug in a condition like OSA. Moreover, prior authorization processes may need to be initiated, where healthcare professionals must first secure permission from the insurer before prescribing the drug.
Zepbound’s journey towards coverage is not isolated; it draws parallels with Novo Nordisk’s Wegovy, which has similarly been granted coverage under Medicare for its approved indications related to cardiovascular risk. Both medications underscore a shifting paradigm within the healthcare industry, where the synergistic relationship between obesity and other comorbidities is gaining recognition. While both companies actively investigate further applications for their drugs—including treatments for chronic kidney disease and fatty liver disease—these applications would first need to navigate rigorous clinical trial processes before obtaining FDA endorsement.
Notably, the Medicare landscape remains complex, as drugs like Ozempic and Mounjaro—indications for diabetes—garner broader coverage, showcasing a nuanced approach based on specific health conditions. This creates an uneven playing field for patients managing obesity alongside other health issues, highlighting systemic disparities that need addressing.
The framework surrounding Medicaid coverage for Zepbound introduces yet more layers of variability. Coverage hinges not only on the prescribed condition but also on the manufacturer’s agreement with the program. If Zepbound is prescribed for obstructive sleep apnea, then coverage may follow if Eli Lilly honors its Medicaid drug rebate agreement. In contrast, if the drug is prescribed purely for weight loss, the state Medicaid programs possess the right to decline coverage, reflecting deeper systemic issues that introduce inconsistency in patient access across different states.
The impending proposal from the Biden administration, designed to widen Medicare and Medicaid access to weight loss drugs, has garnered both attention and concern. Estimates suggest that this initiative could dramatically increase costs, projecting expenses of up to $35 billion over the next decade. The political and economic ramifications of this potential policy are significant, as they potentially reshuffle how medications for obesity could be incorporated into treatment plans.
The recent move to include Zepbound under Medicare coverage for OSA is a promising but complicated step toward addressing obesity and its interconnected health challenges. As healthcare policymakers grapple with the cost implications and equitable access to obesity medications, patients must navigate a complex landscape where access to potentially life-altering treatments hinges on regulatory and administrative structures.
Future discussions around obesity drugs must continue to integrate the multifaceted roles they play in treating comorbid conditions, ensuring that the healthcare infrastructure evolves in a way that prioritizes patient health outcomes while balancing economic constraints. As both political and medical communities engage in these dialogues, the impact on millions of Americans struggling with weight management and related health challenges remains central to the conversation.

Leave a Reply