The herpes simplex virus type 1 (HSV-1) is universally recognized for causing cold sores, but recent research unveils a more insidious aspect of this ubiquitous virus: its potential implications for brain health and neurodegenerative diseases. A collaborative study conducted by scientists from the University of Colorado and the University of Bourgogne delves into how HSV-1 interacts with various brain regions, thereby broadening our understanding of its influence on neurological conditions, including Alzheimer’s disease.
Traditionally viewed as a superficial affliction, HSV-1 is now understood to have the capability of infiltrating deeper structures of the body, notably the central nervous system (CNS). The pathways for this invasion predominantly involve the trigeminal and olfactory nerves. However, the mechanisms of how the virus disseminates through the brain remain an area of active inquiry. Clarifying these pathways is critical, as neuroscientist Christy Niemeyer articulates the necessity of identifying the vulnerable brain regions affected by HSV-1 to comprehend how this virus could precipitate chronic neurological diseases.
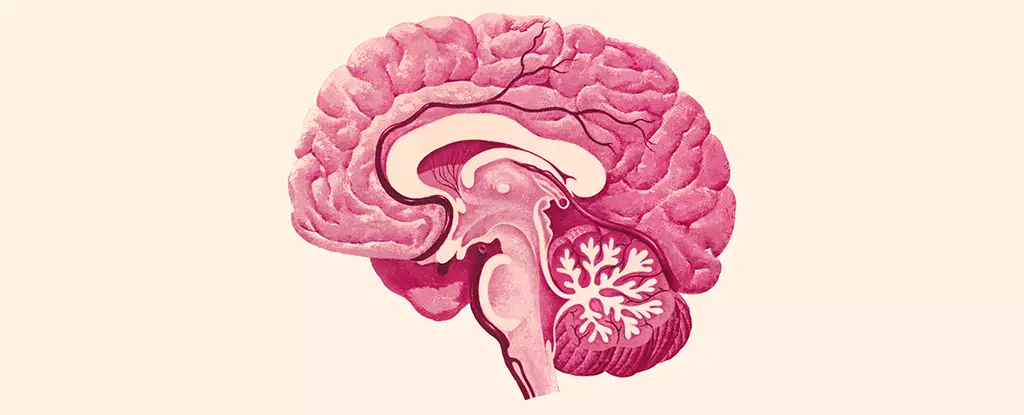
The study meticulously charted the territories of the brain compromised by HSV-1 infection. Notably, areas such as the brainstem and hypothalamus surfaced as primary targets. The brainstem plays a crucial role in fundamental bodily functions like heart rate and respiratory control, while the hypothalamus governs hormonal balances, moods, and sleep cycles. The repercussions of HSV-1’s presence in such pivotal regions fuel a dire need for a deeper understanding of the virus’s neuropathological consequences.
Microglia, the primary immune cells in the brain, were observed to mount inflammatory responses upon HSV-1 infection. This inherent immune reaction was substantial, creating a state of persistent activation even after the viral presence diminished, indicating possible long-term ramifications for brain function. The chronic inflammation engendered by the activated microglia could initiate a cascade of neurodegenerative changes, corroborating the hypothesis that untreated infections may pave the way for conditions like Alzheimer’s.
While the study did not escalate to full-blown cases of encephalitis, where broader brain inflammation could lead to critical health crises, the findings suggest that even localized infections could diminish functionality in the affected regions. Therefore, the relationship between viral infection and neurodegenerative processes intensifies, marking a pressing area for future research.
In the scope of recent scientific inquiries, HSV-1 has been increasingly scrutinized for its correlation with various neurodegenerative disorders, prominently Alzheimer’s disease. While the precise pathways linking HSV-1 to Alzheimer’s remain ill-defined, the overlapping impacts on critical brain regions present a substantive platform for hypothesis. The affected areas, particularly those involved in memory and cognition, highlight an alarming intersection that may underpin the mechanisms by which chronic infections exacerbate neurological decline.
Researchers have posited that the intricate interplay of HSV-1 and inflammatory responses from microglial cells may serve as crucial factors contributing to the onset and progression of Alzheimer’s disease. As chronic inflammation is a recognized trigger for neurodegenerative diseases, understanding how HSV-1 perpetuates this inflammatory cycle could unveil novel preventative strategies or therapeutic targets.
As the study provides substantial insights into the relationship between HSV-1 and neurological health, it sparks further inquiry into treatment protocols and preventive measures. The need for targeted research aimed at untangling the complexities of HSV-1 infection within the CNS is crucial. Exploring the potential of anti-viral therapies to mitigate the post-infection inflammatory responses could lead to significant advancements in dementia care and prevention.
This evolving narrative emphasizes the significance of distinguishing the multifaceted roles infectious agents like HSV-1 play in brain health. Future studies must continue to bridge the gaps in understanding these viral-inflammation interactions and their implications for diseases like Alzheimer’s, ultimately guiding clinical practices toward improved patient outcomes. The link between a common virus and severe neurological implications exemplifies the necessity for ongoing exploration in this critical area of neuroscience.

Leave a Reply