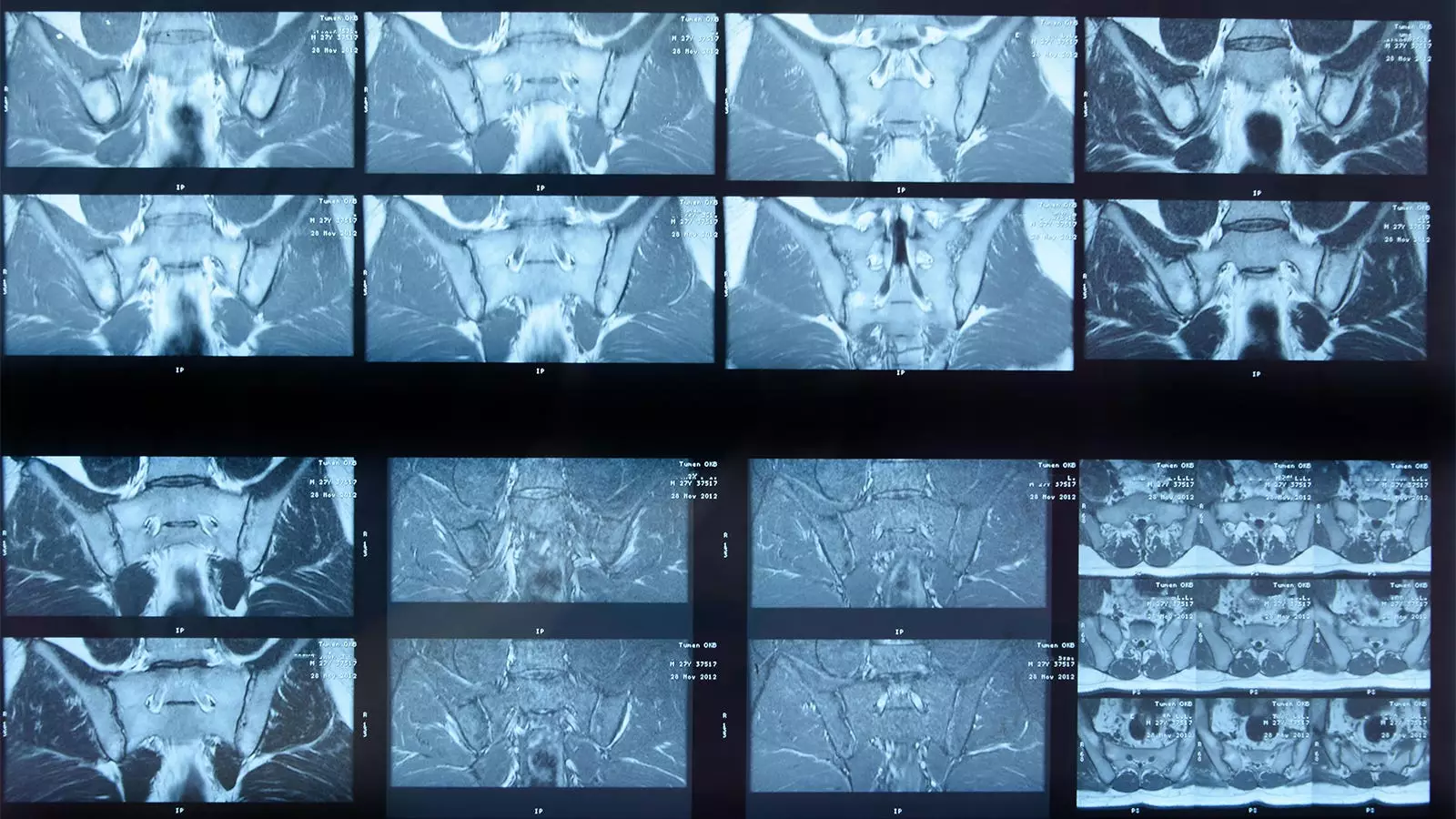
The integration of artificial intelligence (AI) into medical diagnostics has shown promise, particularly in the realm of imaging technologies. One such technological advancement includes a deep learning algorithm specifically designed to analyze MRI scans for signs of inflammation in the sacroiliac joints (SIJs) of patients diagnosed with axial spondyloarthritis (axSpA). This article aims to delve deeper into a recent study that examined the effectiveness of this AI system in comparison with expert human readers.
Study Overview and Findings
Research led by Joeri Nicolaes, PhD, and colleagues at UCB Pharma analyzed MRI scans from 731 axSpA patients to assess the algorithm’s performance. The study hypothesized that the AI’s findings would correlate closely with those of a panel of expert readers. In their analysis, both methods identified SIJ inflammation in 304 cases and agreed on the absence of inflammation in another 239 instances. However, the researchers also encountered discrepancies where human experts detected inflammation overlooked by the AI, totaling 132 images. The AI, conversely, flagged inflammation in 56 instances that experts deemed negative.
The statistics presented are worth examining closely. The system achieved a 74% absolute agreement rate with human readers, demonstrating that while the AI’s performance could be labeled as “acceptable,” it still falls short of the benchmarks often expected in clinical settings. The sensitivity, specificity, and predictive values highlight areas for potential improvement: a sensitivity of 70% signifies that a sizeable portion of inflamed cases went undetected by the AI, while a negative predictive value of 64% raises concerns about its reliability in ruling out the disease.
While these results present a relatively cautious view of the algorithm’s clinical utility, it is pertinent to contextualize these findings. The researchers acknowledged that the strict criteria for confirming inflammation (requiring involvement of at least two SIJs) may have skewed results against the algorithm. Moreover, the expert panel’s collective insights were likely influenced by additional clinical parameters outside the MRI images, factors that the AI could not incorporate, thereby leading to potential biases in detection.
Interestingly, the study underscores how the depth of expertise among the human readers may outstrip that of general practitioners, capturing a unique perspective on the potential role of AI in settings where expert interpretation might be absent. In scenarios where instant interpretations are necessary, AI could serve as a valuable initial screening tool, facilitating timely clinical decision-making.
A notable advantage of AI algorithms lies in their ability to produce reproducible results, an aspect that contrasts sharply with human interpretation, which may be affected by factors such as fatigue, differing levels of experience, and personal biases. In this regard, incorporating AI systems into clinical workflows could help to standardize evaluations of SIJ inflammation, ensuring that practitioners can make decisions based on consistent diagnostic data.
Nevertheless, the authors caution against over-reliance on AI technology. Variance in reader decisions—be it between different human experts or even the same individual on separate occasions—may result in missed diagnoses or over-diagnoses. Therefore, the implementation of such algorithms should be viewed as complementary to human expertise rather than a replacement.
Limitations and Future Directions
Several limitations impact the applicability of the AI algorithm in everyday clinical practice. The lack of capability to detect structural damage from MRI scans diminishes its utility, as clinicians often rely on this critical element for effective treatment planning. Furthermore, a considerable number of patient scans could not be processed due to technical incompatibilities, thereby limiting the dataset and potentially introducing bias in the algorithm’s performance evaluation.
As classification criteria for SIJ inflammation evolve over time, an imperative exists to update the algorithm’s design accordingly. Future iterations should focus on enhancing sensitivity and applicability, ensuring the AI can operate effectively even in the presence of diverse imaging conditions.
While the study presents a cautious yet optimistic outlook on an AI algorithm for MRI scanning in axSpA, it simultaneously highlights the technology’s limitations and the continuing necessity for expert interpretation. As AI continues to advance in the realm of medical imaging, collaborative efforts between technology and human expertise will be essential to improve diagnostic accuracy and patient outcomes. The potential of AI in healthcare exists, but its integration must be carefully considered to leverage its capabilities effectively while still valuing the critical insights human specialists provide.

Leave a Reply